Welcome
General Practice Assistants (GPAs)
Overview of role
As part of the wider team in general practice, general practice assistants provide a support role, carrying out administrative tasks, combined in some areas with basic clinical duties.
They can help to free up GP’s time and contribute to the smooth running of appointments, improving patients experience in the surgery.
The focus being on supporting general practitioners in their day-to-day management of patients, specifically aimed at reducing the administrative burden, making best use of consultation time and supporting those particularly vulnerable to isolation who are regular attenders at the practice.
This video features the new medical assistant role.
Evidence of success
Evidence suggests that effective adoption of this role has the potential to:
- improve patient access and release highly qualified staff to concentrate on treating and managing patients with more complex conditions (HEE GPA Working Group Report 2018)
- improve patient flow within surgery hours, increasing the time efficiency of appointments, and reduction of waiting times; supporting patient experience by ‘translating’ or reiterating information from the GP (University of Cumbria 2017)
- have a positive impact on GP retention and job satisfaction
- reduce time spent by GPs on managing correspondence by 85% (Surrey Heath Community Providers, 2018).
Evidence and benefits – GPA-Evidence-and-Benefits.pdf (e-lfh.org.uk)
Accredited GPA training programme
Some of our BSOL GPAs have previously completed a GPA accredited course when this was introduced as a pilot. This is now being delivered nationally. There are limited spaces available on current accredited training programmes through the University of Derby and apprenticeship programmes supported by Lincolnshire Training Hub (Midlands GPA Programme – Lincolnshire Training Hub) who are managing the GPA accredited course route on behalf of all Midlands Training Hubs. BSol Training Hub will support where we can and will provide the three clinical training sessions on behalf of Lincolnshire in phlebotomy, basic clinical skills and wound care.
If more spaces become available, or if a further course is introduced, BSol Training Hub will be in touch with more information.
Non accredited portfolio route
As spaces on the accredited training course and apprenticeship course are so limited; it is accepted nationally that GPA’s can work towards their competencies and build their own portfolio with in-practice training and support from a GP mentor. Capabilities and portfolio are the same as if completed via a training programme and competencies should be signed off by the GP mentor responsible. Whilst the portfolio does not need to be submitted to an external agency; it should be completed and the GPA should be working within these capabilities as they have competency to do so. This will be managed by the GPA and their GP mentor and should be documented and signed by each once competencies and capabilities are assessed and confirmed.
Additional roles reimbursement scheme (ARRS)
The GP Assistant role is reimbursable via the Additional Roles Reimbursement Scheme (ARRS). If the role is reimbursed via ARRS, please note the following requirements as documented in the NHS England 2023/2024 Direct Enhanced Specification – Click here to view a copy of the DES
The Network DES is a contract adhered to by Primary Care Networks. The DES contains specific information and requirements for the additional roles reimbursement scheme (ARRS).
These are the specifications for the GPA:
B.16 General Practice Assistants
B16.1 General Practice Assistants (GPAs), support the smooth running of clinics by performing more routine administration and clinical tasks on behalf of the GP, freeing up their time to focus on the patient.
B16.2 The role is subject to a maximum reimbursement equivalent of an Agenda for Change band 4 level. Staff can be trained in-practice, with on-job training and development led by GPs, in line with the role outline and national competency framework. Trainee GPAs may also complete HEE’s accreditation programme, aligned to the competency framework, equipping them with formal certification of their learning. These staff are supported by a structured development programme (managed by HEE) and gain formal certification after around nine months.
B16.3 While in post, GPAs are expected to deliver a combination of the following requirements based on their level of skills and experience. PCNs may claim reimbursement for the time GPAs spend delivering these activities, or undertaking training to deliver them: a. arranging appointments, referrals, tests and follow up appointments of patients:
- completing simple clinical observations /investigations as directed locally, such as dipstick urine, taking blood pressure, ECG, phlebotomy
- supporting the GP with immunisations/wound care
- preparing patients prior to going in to see the GP, taking a brief history and basic readings in readiness for the GP appointment
- completing basic (non-opinion) forms and core elements of some forms for the GP to approve and sign such as insurance forms, mortgage, benefits agency forms etc.
- explaining treatment procedures to patients
- helping the GP liaise with outside agencies e.g. getting an on call doctor on the phone to ask advice or arrange admission while the GP can continue with their consultation(s)
- sorting clinical post and prioritising for the GP. Signposting some post to other members of staff
- extracting information from clinical letters that needs coding, adding this to patient notes. Supporting with QOF reviews.
B16.4 GPAs should also:
- Participate in an annual individual performance review.
- Track and record evidence of their experience against the national competency framework.
- Inform the lead GP of any concerns regarding their role and request professional development as needed.
- Be aware of their own professional boundaries and what to do when they are reached.
GPA competency framework
Testing accessibility document (e-lfh.org.uk)
Building-porfolio-evidence-for-elfh.pdf (e-lfh.org.uk)
Supporting-resources-aligned-to-comp-framework.pdf (e-lfh.org.uk)
This competency framework specifies a range of core capabilities expected of the General Practice Assistant (GPA) working within general practice/primary care.
The framework is structured around 5 key domains:
- Care
- Administration
- Clinical
- Communications
- Managing Health Records
Within the domains are a total of 58 capabilities. The capabilities are numbered for ease of reference – this does not indicate a prescribed pathway, process or hierarchy.
The capabilities set out what the GPA working in general practice/primary care settings should demonstrate.
To further support GP practices in identifying and reviewing capabilities, specific assessment criteria has also been included in the framework.
This will help GPAs to build a portfolio of evidence and demonstrate the required knowledge, skills and behaviours essential to the GPA role, and promote clinical thinking and reflection.
The portfolio capabilities are included in the link above. All GPA’s should be working towards achieving all competencies and should be recording evidence and skills learnt and demonstrated. Training to support with elements of this will be provided by the BSol Training Hub, however all competencies need to be signed off by the GP mentor who remains responsible for the GPA
Patient Education
Keep the patients informed about the new/changing members of your team.


Clinical Supervision
All GPA’s require clinical supervision. All GPA’s must have an assigned GP Mentor. When the GP Mentor is not in practice another suitable member of the team should be allocated as a supervisor for the GPA.
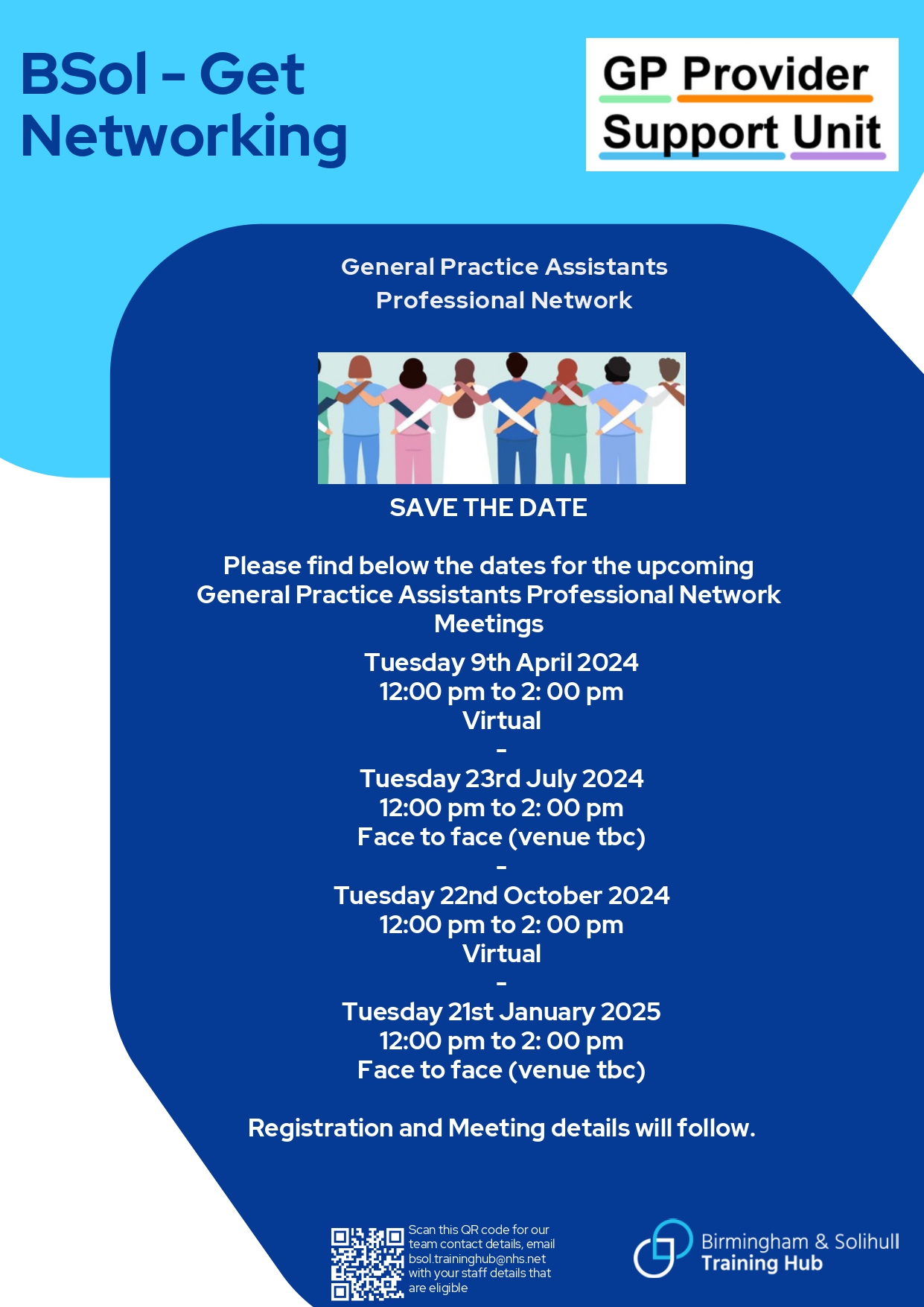
GPA Professional Network
We have established a professional network for the General Practice Assistants working in BSol in collaboration with the BSol GP Provider Support Unit.
The Professional Networks are chaired by our Training Hub Ambassadors/ Facilitators or a member of the network. Meetings are held on a quarterly basis and are a combination of face to face and virtual meetings.
The meetings will:
- Provide a safe space for members of the team to come together for peer support and networking.
- Be a platform to discuss best practice, ways of working and projects.
- Provide updates relating to the role.
- Provide role specific training
- Help members of the team to promote the benefits of the role for both staff and patients.
If you have not registered your details to receive communications about the professional network, or if you are new to the role, please contact us so that we can add you to our mailing list and send you the meeting invites.
Email – bsol.traininghub@nhs.net
GPA WhatsApp Group
We have a WhatsApp group for GPA’s. If you would like to be a part of this WhatsApp group please complete the short form using this link: GPA Whatsapp Group Consent Form (google.com)
Please note that the GPA Whatsapp group is for GPAs working in Birmingham and Solihull only. There are other forms of communication for other roles – please view the relevant website page to see what is available for each role, or email us at bsol.traininghub@nhs.net.
By completing this form you consent to your details being held on record by BSol Training Hub. Details will never be shared without your express consent to do so.
This is a professional working group. Please ensure that all conversations are work related and respectful to your colleagues.
The administrators of this WhatsApp group reserve the right to remove members that share inappropriate content.
As part of our information governance responsibilities we are required to remind members of the purpose of the group which is to discuss and share relevant professional information.
Please consider the following:
Whilst most of the guidance or information provided by colleagues is relevant and accurate, we do not provide governance of it so sourcing response through these established routes is essential to maintain safe practice.
Frequently Asked Questions
Please refer to the frequently asked questions document that has been created to support Primary Care Networks (PCNs), Training Hubs, GP practices and other primary care colleagues click here to view






















